
STROLL THROUGH THE SECOND EXHIBIT
Journey through the clinical manifestations of PsA
PsA=psoriatic arthritis.
PsA is a chronic autoimmune inflammatory disease of the skin and musculoskeletal system…
…characterized by systemic inflammation.1

LECTURE SERIES WITH DR. SAAKSHI KHATTRI
Get insights on the importance of recognizing PsA earlier
Join Dr. Saakshi Khattri, acclaimed physician and educator in the fields of dermatology and rheumatology, as she discusses the importance of listening to patients and how diagnosing PsA earlier can help avoid irreversible damage.
Progression to PsA
PSO and PsA are distinct conditions but share clinical features.1
In over 70% of cases, PSO will precede PsA; however2:
- 10%–15% of patients can present with PsA preceding PSO1
- 13% of cases present with joint symptoms preceding the onset of skin symptoms3
- 21% of cases present with a parallel onset of skin and joint involvement1
Many factors have been identified to contribute to the progression of chronic inflammation over time, including environmental, genetic, and molecular events.4

The domains of PsA
PsA results in several articular and extra-articular manifestations, which can be grouped into 6 domains based on the site affected5:
- Peripheral arthritis
- Enthesitis*
- Dactylitis*
- Axial disease
- Nail disease
- Skin disease
Additional manifestations of PsA include:
- uveitis
- IBD6
*Caused by peripheral joint inflammation.
IBD=inflammatory bowel disease.
Many PsA patients present with multiple disease domains6,†
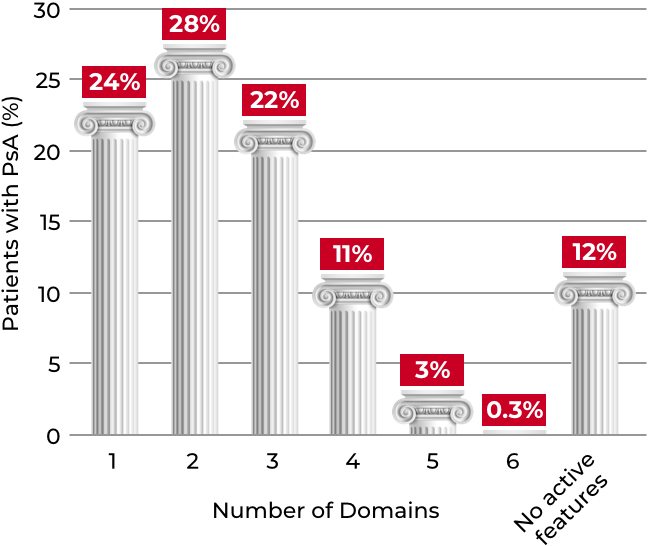
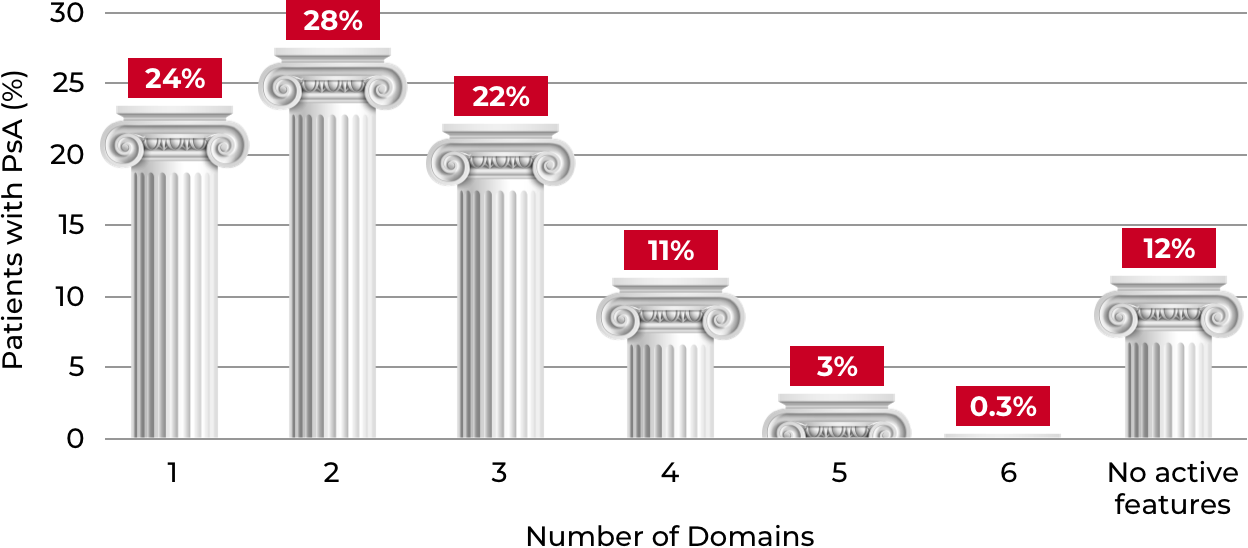
Most PsA patients present with multiple domain manifestations, reflecting the heterogeneity of disease presentation. The most common single-domain and multidomain presentations are skin disease and peripheral arthritis + skin disease, respectively.6
†Data from adults with PsA (N=2617) enrolled in the Corrona PsA/SpA Registry (March 2013-August 2018). Six PsA disease domains were evaluated: enthesitis, dactylitis, peripheral arthritis, nail psoriasis, axial disease, and skin disease.6
The unique features of axSpA vs axial PsA7
axSpA
- Demographic
-
More frequent in younger ages and more common in men
- Clinical
-
More inflammatory back pain and less peripheral involvement
- Imaging
-
- Symmetrical sacroiliitis
- More symmetrical and marginal syndesmophytes
- Lumbar joints are commonly involved
- Genetic
-
Frequently associated with HLA-B27 (90%)
Axial PsA
- Demographic
-
More frequent in older ages and similar frequency in men and women
- Clinical
-
Less inflammatory back pain and more peripheral involvement
- Imaging
-
- Asymmetrical sacroiliitis
- Less symmetrical and non-marginal syndesmophytes with paravertebral ossification
- Cervical joint involvement
- Genetic
-
Frequently associated with HLA-B08 and HLA-B38 (90%), less frequently with HLA-B27 (14%–44%)
axSpA=axial spondyloarthritis; HLA=human leukocyte antigen.
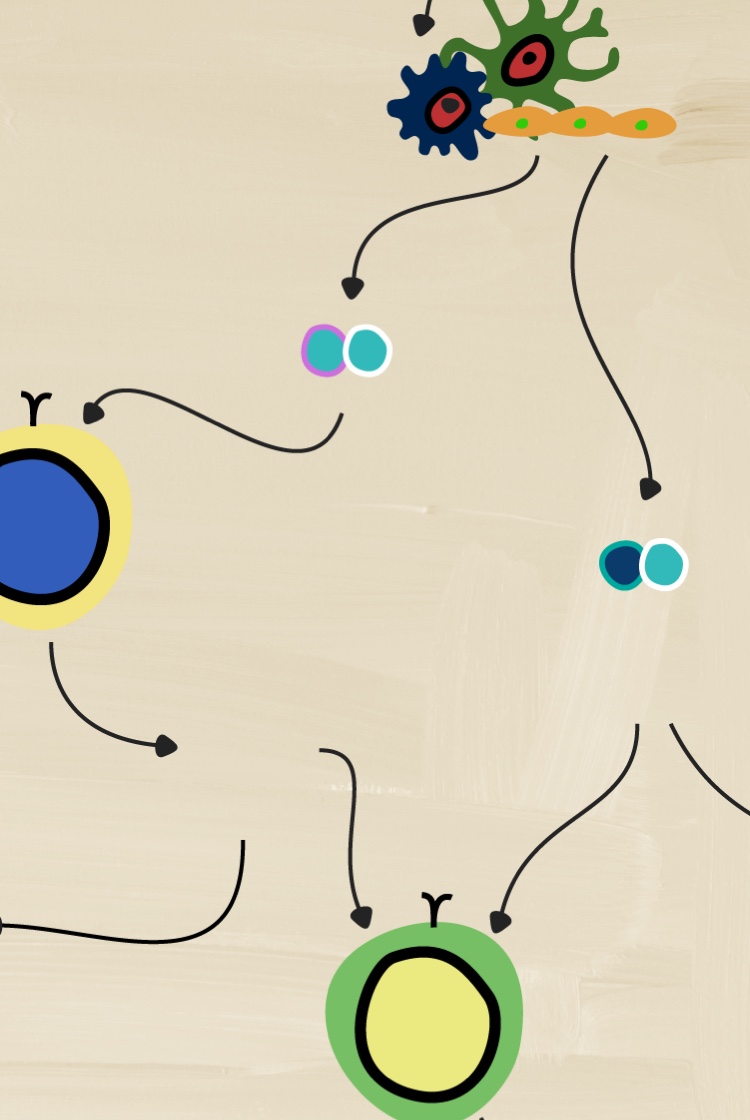

How does pathobiology factor into the complexity of inflammation?
Discover how several different cytokines have distinct roles in driving inflammation that leads to disease processes.


NEXT ROOM IN THE MANIFESTATIONS EXHIBIT
Clinical manifestations
Review the important distinctions that are emerging about which cytokines contribute to the various clinical manifestations of PsA.
PREVIOUS ROOM
PsA pathobiology
Become a member of the RheuMuseum and be the first to know about new exhibits
- Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74(4):423-441. doi:10.1007/s40265-014-0191-y
- Giovannini I, Bosch P, Dejaco C, et al. The digital way to intercept psoriatic arthritis. Front Med (Lausanne). 2021;8:792972. Published 2021. doi:10.3389/fmed.2021.792972
- Kumar R, Sharma A, Dogra S. Prevalence and clinical patterns of psoriatic arthritis in Indian patients with psoriasis. Indian J Dermatol Venereol Leprol. 2014;80(1):15-23. doi:10.4103/0378-6323.125472
- Scher JU, Ogdie A, Merola JF, et al. Preventing psoriatic arthritis: focusing on patients with psoriasis at increased risk of transition. Nat Rev Rheumatol. 2014;15(3):153-166. doi:10.1038/s41584-019-0175-0
- Ogdie A, Rozycki M, Arndt T, et al. Longitudinal analysis of the patient pathways to diagnosis of psoriatic arthritis. Arthritis Res Ther. 2021;23:252.doi: 10.1186/s13075-021-02628-2
- Ogdie A, Hur P, Liu M, et al. Effect of multidomain disease presentations on patients with psoriatic arthritis in the corrona psoriatic arthritis/spondyloarthritis registry. J Rheumatol. 2021;48(5):698-706. doi:10.3899/jrheum.200371
- Poddubnyy D, Jadon DR, Van den Bosch F, et al. Axial involvement in psoriatic arthritis: An update for rheumatologists. Semin Arthritis Rheum. 2021;51(4):880-887. doi:10.1016/j.semarthrit.2021.06.006