

STROLL THROUGH THE SECOND AXSPA EXHIBIT
Journey through axSpA manifestations
axSpA=axial spondyloarthritis.
In this exhibit,
you’ll explore the
clinical features and manifestations of axSpA…
…its burden of disease
and the impact on patients’ quality of life.

LECTURE SERIES WITH DR. SAAKSHI KHATTRI
Get insights on the importance of recognizing axSpA earlier
Watch the first video in a series featuring Dr. Saakshi Khattri, acclaimed physician and educator in both dermatology and rheumatology, as she discusses the importance of listening to patients and the risks of delayed axSpA diagnosis.
The classification of SpA
AxSpA belongs to a group of inflammatory rheumatic diseases, called SpA, which share overlapping clinical and genetic features.1
Two SpA types are distinguished1:
- Axial SpA (axSpA)—predominantly affects the axial skeleton
- Peripheral SpA—predominantly affects peripheral joints
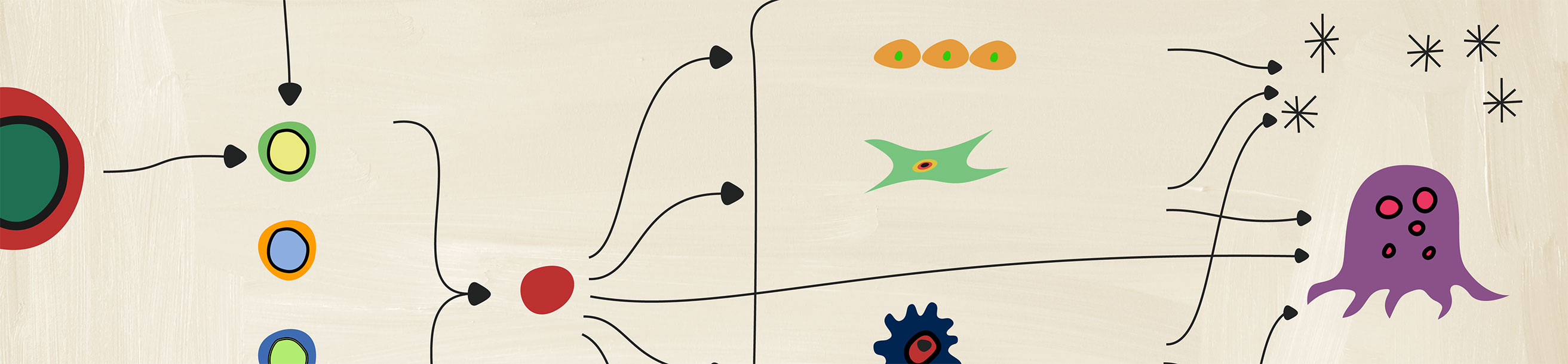
The overlapping SpA subgroups2
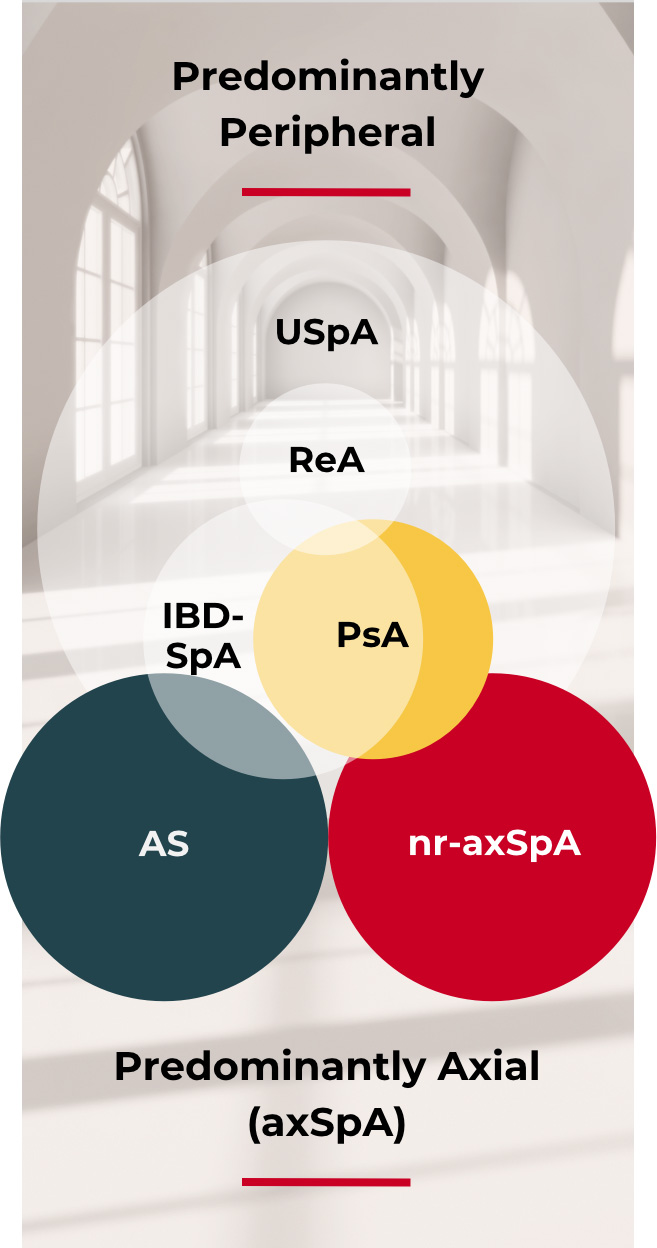
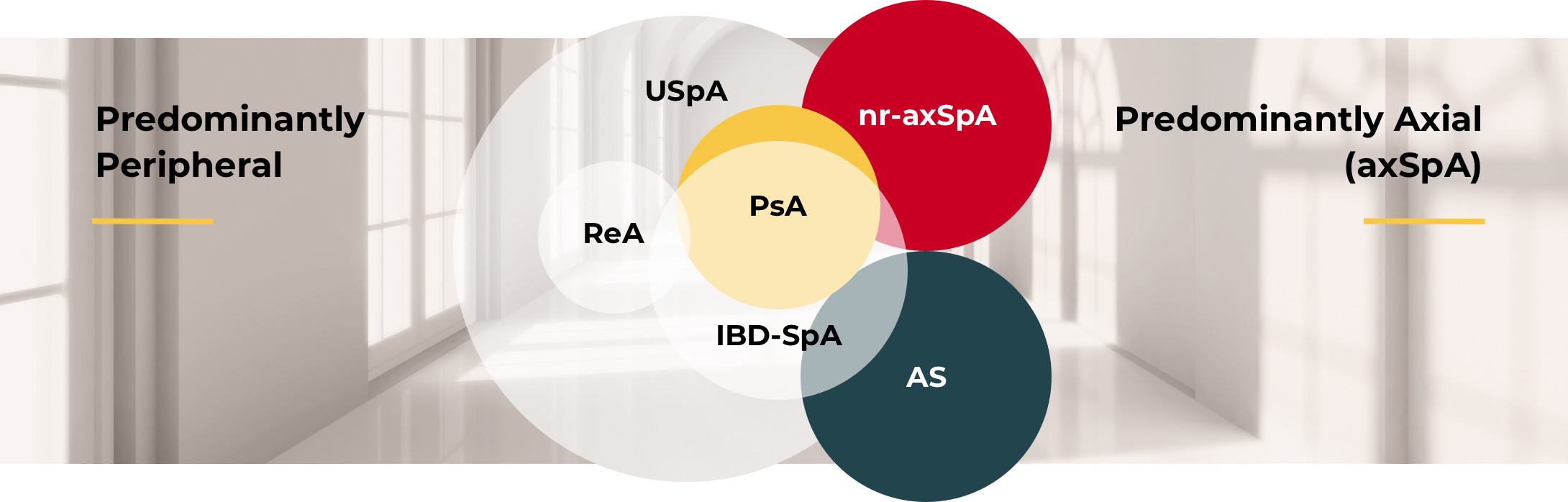
© Reprinted from Raychaudhuri SP and Deodhar A. The classification and diagnostic criteria of ankylosing spondylitis. J Autoimmun. 2014;48-49:128-133, with permission from Elsevier.
AS=ankylosing spondylitis; IBD-SpA=inflammatory bowel disease and spondyloarthritis; nr-axSpA=non-radiographic axial spondyloarthritis; ReA=reactive arthritis; SpA=spondyloarthritis; USpA=undifferentiated spondyloarthritis.
Features of nr-axSpA and AS
A combination of SpA features* and imaging distinguishes nr-axSpA from AS.1,3
The clinical diagnosis of axSpA is often informed by imaging findings.4 axSpA can be divided into two subgroups, nr-axSpA and AS (also called radiographic axSpA), based on evidence of radiographic sacroiliitis by mNY grading.3,†
nr-axSpA†


AS


*SpA features include inflammatory back pain, arthritis, enthesitis (heel), uveitis, dactylitis, psoriasis, Crohn’s disease/ulcerative colitis, good response to NSAIDs, family history of SpA, HLA-B27, and elevated CRP.3
†As defined by ASAS classification criteria (note that classification criteria, but not diagnostic criteria, are available for axSpA and it is important not to use classification criteria for diagnostic purposes).5
ASAS=Assessment of SpondyloArthritis international Society; CRP=C-reactive protein; mNY=modified New York; NSAIDs=nonsteroidal anti-inflammatory drugs.
Burden of disease
Misconception persists that all nr-axSpA patients progress to AS; however, one study showed that only ~60% of patients with nr-axSpA progress to AS over a 10-year period.1 This occurs when inflammation in sacroiliac joints leads to structural changes that are detectable on a radiograph.1
Without associated X-ray imaging, patients with nr-axSpA are often misdiagnosed and their condition improperly assessed as a mild form of disease.6
Patients with nr-axSpA or AS experience an equal burden of disease, which includes1:
- Pain
- Stiffness
- Fatigue
Prevalence based on gender
axSpA often affects men and women who are under age 40.7,8 However, there are gender disparities across nr-axSpA and AS, including prevalence, time to diagnosis, and disease manifestations, thought to be driven by different immunological, hormonal, and genetic responses.9 nr-axSpA is generally more prevalent in women (53%) versus men (47%) and AS is more prevalent in men (70%) versus women (30%).10
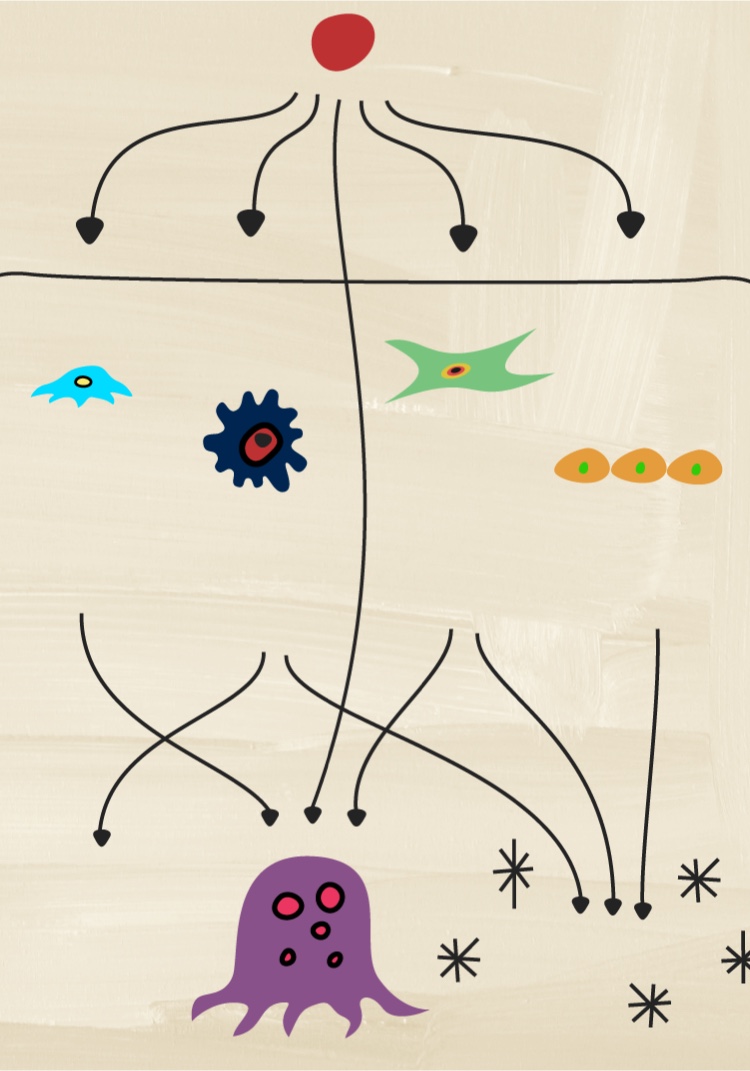
How does pathobiology factor into the complexity of inflammation?
Discover how several different cytokines have distinct roles in driving inflammation that drives disease processes.


NEXT ROOM IN THE MANIFESTATIONS EXHIBIT
Clinical manifestations
Visit the hall of statues to explore the various clinical manifestations of axSpA
PREVIOUS EXHIBIT
axSpA pathobiology
Become a member of the RheuMuseum and be the first to know about new exhibits
- Sieper J, Braun J, Dougados M, et al. Axial spondyloarthritis. Nat Rev Dis Primers. 2015;1:15013
- Raychaudhuri SP, Deodhar A. The classification and diagnostic criteria of ankylosing spondylitis. J Autoimmun. 2014;48-49:128-33. doi: 10.1016/j.jaut.2014.01.015.
- Robinson PC, van der Linden S, Khan MA, et al. Axial spondyloarthritis: concept, construct, classification and implications for therapy. Nat Rev Rheumatol. 2021;17:109-118.
- Michelena X, López-Medina C, Marzo-Ortega H. Non-radiographic versus radiographic axSpA: what's in a name? Rheumatology (Oxford). 2020;59(Suppl4):iv18-iv24. Published 2020. doi: 10.1093/rheumatology/keaa422.
- Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68:777-783.
- Ghosh N, Ruderman EM. Nonradiographic axial spondyloarthritis: clinical and therapeutic relevance. Arthritis Res Ther. 2017;19(1):286.
- Rudwaleit M, Haibel H, Baraliakos X, et al. The early disease stage in axial spondylarthritis: results from the German Spondyloarthritis Inception Cohort. Arthritis Rheum. 2009;60(3):717-727. doi:10.1002/art.24483
- Burgos-Varga R, Wei JC, Rahman MU, et al. The prevalence and clinical characteristics of nonradiographic axial spondyloarthritis among patients with inflammatory back pain in rheumatology practices: a multinational, multicenter study. Arthritis Res Ther. 2016;18(1):132.
- Rusman T, van Vollenhoven RF, van der Horst-Bruinsma IE. Gender differences in axial spondyloarthritis: women are not so lucky. Curr Rheumatol Rep. 2018;20(6):35.
- de Winter JJ, van Mens LJ, van der Heijde D, et al. Prevalence of peripheral and extra-articular disease in ankylosing spondylitis versus non-radiographic axial spondyloarthritis: a meta-analysis. Arthritis Res Ther. 2016;18(1):196. doi:10.1186/s13075-016-1093-z